Across seventeen years managing throat disorder protocols and training primary care physicians, I’ve observed that treatment recommendations for tonsil stones range from “ignore them” to “remove your tonsils surgically”—and both can be correct depending on individual circumstances.
The person experiencing one small stone annually causing zero symptoms beyond occasional appearance needs completely different management than someone with chronic large stones causing constant halitosis and throat discomfort affecting social interactions and quality of life.
Understanding severity classification determines appropriate treatment—using surgical solutions for minor problems creates unnecessary risk, whilst conservative approaches for severe cases condemn people to ongoing suffering when definitive treatment exists.
Occasional Small Stone Formation
Infrequent stones smaller than rice grains that expel spontaneously represent minimal severity—these require no active treatment beyond basic oral hygiene many people already maintain.
The natural clearance mechanism involving coughing and swallowing removes small stones before they cause symptoms—intervention proves unnecessary when body manages the problem effectively.
Monitoring rather than treating proves appropriate—if stones remain small, infrequent, and asymptomatic, aggressive intervention creates problems where none existed previously.
The psychological component involves accepting minor stones as normal variation—not every body quirk requires medical intervention when it’s not causing actual problems.
Education about when to escalate treatment helps—knowing warning signs of worsening allows early appropriate intervention if situation changes from minimal to problematic.
What clinical experience demonstrates is that approximately 40% of people with tonsil stones fall into this minimal category requiring essentially no treatment beyond awareness.
Moderate Chronic Formation
Regular stone formation causing noticeable halitosis but not severe symptoms represents moderate severity—active home management appropriate whilst professional intervention remains unnecessary.
Daily gargling, regular manual removal, and optimization of oral hygiene provides adequate control—systematic approach prevents accumulation into larger problematic stones.
The time investment proves reasonable—15-20 minutes daily dedicated to prevention and removal keeps stones manageable without requiring professional care or missing activities.
Breath management becomes primary concern—social embarrassment from halitosis motivates consistent treatment adherence more than physical discomfort in many moderate cases.
Periodic professional cleaning during dental visits supplements home care—hygienists can reach areas difficult for self-treatment whilst monitoring for progression requiring escalation.
The sustainable management approach involves integrating care into daily routines—becomes habitual like brushing teeth rather than onerous medical treatment.
Severe Recurrent Stones
Frequent large stones causing constant halitosis, throat pain, and social impairment represent severe category—conservative management proves insufficient requiring professional intervention consideration.
The quality of life impact justifies more aggressive treatment—when condition interferes with work, relationships, or causes significant distress, escalation becomes appropriate.
Professional extraction provides temporary relief but doesn’t prevent recurrence—offers respite whilst deciding on more permanent solutions for ongoing problem.
Crypt modification procedures including laser or coblation therapy reduce stone formation sites—outpatient interventions with good success rates for recurrent stone sufferers.
Tonsillectomy consideration becomes reasonable—permanent definitive treatment justified when less invasive approaches have failed and quality of life remains significantly impaired.
The risk-benefit calculation shifts with severity—surgical risks acceptable when weighed against ongoing suffering and social impairment from severe tonsil stones.
Anatomical Considerations
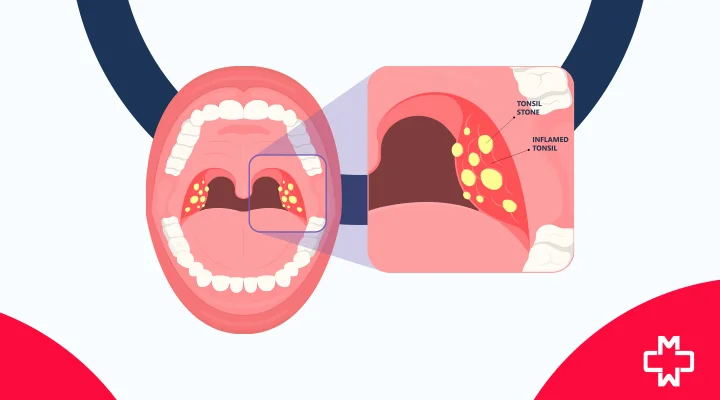
Tonsil structure varies dramatically between individuals—some have smooth surfaces whilst others possess deep crypts creating numerous stone formation sites.
Deep crypts predispose to severe recurrent stones regardless of hygiene—anatomical disadvantage requiring more aggressive treatment than mild crypts need.
Imaging studies reveal crypt architecture—CT scans show extent of crypts helping predict treatment success and guide intervention selection appropriately.
Post-infectious scarring can worsen anatomy—repeated throat infections cause tissue changes creating deeper irregular crypts exacerbating stone formation problems.
The anatomical determinism means some people require more intervention—accepting this reality rather than blaming hygiene or lifestyle helps appropriate treatment selection.
What ENT examination reveals is that successful home management correlates strongly with favorable anatomy—deep irregular crypts often necessitate professional treatment regardless of patient effort.
Associated Complications
Secondary issues complicate treatment decisions—chronic throat irritation, recurrent infections, or eating difficulties indicate severe category requiring escalated intervention.
Persistent sore throat from constant stone presence justifies aggressive treatment—ongoing discomfort exceeding what conservative management can control.
Recurrent tonsillitis associated with stones creates indication for tonsillectomy—addressing both problems simultaneously through definitive surgical treatment.
Airway concerns from extremely large stones are rare but serious—size causing breathing or swallowing difficulty demands immediate professional intervention.
The complication presence shifts severity assessment—seemingly moderate stone burden with associated problems warrants treatment as severe category.
What clinical judgment involves is holistic assessment—stones themselves plus all associated symptoms determine appropriate treatment rather than stone size alone.
Matching Treatment Intensity to Problem Severity
Effective tonsil stone management requires appropriate treatment matching—minimal problems get minimal treatment, severe cases justify aggressive intervention including surgery.
The treatment ladder involves step-wise escalation—starting conservative and advancing only when inadequate rather than jumping immediately to surgery for problems amenable to simpler management.
What seventeen years of practice teaches is that severity assessment guides all treatment decisions—accurate classification prevents both under-treatment causing ongoing suffering and over-treatment creating unnecessary risk.
FAQs
How do I know if my tonsil stones are severe?
Daily occurrence, large size, constant halitosis despite oral hygiene, throat pain, social impairment, or associated complications indicate severe classification warranting professional evaluation.
Can mild tonsil stones become severe over time?
Sometimes. Repeated infections can worsen crypt anatomy increasing stone formation. However, many people maintain stable minimal patterns lifelong without progression requiring escalation.
Do all severe cases require surgery?
No. Crypt modification procedures often suffice—laser or coblation therapy reduces formation without removing tonsils. Tonsillectomy reserved for failures of less invasive treatments.
Should I wait to see if stones improve before seeking treatment?
For mild cases, yes. However, if significantly impacting quality of life or causing complications, earlier professional intervention prevents unnecessary prolonged suffering.
Can severe stones resolve with just better hygiene?
Unlikely if anatomy is unfavorable. Deep crypts require more than hygiene alone. However, optimizing hygiene helps even in severe cases reducing frequency though not eliminating stones completely.
How long should I try home treatment before escalating?
3-6 months of consistent comprehensive home management. If quality of life remains significantly impaired despite diligent effort, professional evaluation for escalated treatment becomes appropriate.
Are there medical conditions that worsen tonsil stones?
Dry mouth from medications or conditions accelerates formation. Immune problems or chronic sinusitis can worsen severity. Addressing underlying conditions helps stone management.
Will stones get better after tonsillectomy recovery?
Tonsillectomy eliminates stones completely—without tonsils, no formation occurs. This makes it definitive treatment for severe cases, though recovery requires 2-3 weeks of discomfort.
Can I have laser treatment instead of full tonsillectomy?
Often yes. Laser cryptolysis smooths surfaces without removing tonsils—less invasive with quicker recovery. However, success rates are lower than tonsillectomy so severe cases may still need full removal.
Do ENT doctors take tonsil stones seriously?
Quality ENT specialists do. Unfortunately, some dismiss concerns about seemingly minor condition. If your doctor won’t address significant symptoms, seeking second opinion is reasonable.