I messed around with home remedies for tonsil stones for three months before finally seeing a doctor. Kept thinking I could handle it myself – gargling, water flossing, trying every internet suggestion. Meanwhile, the problem kept getting worse.
The turning point came when I couldn’t dislodge a particularly large stone that was causing constant pain. My throat hurt, swallowing was difficult, and the bad breath was affecting my confidence at work. Finally admitted I needed professional help.
What I learned is that there’s a clear line between problems you can manage at home and situations requiring medical expertise. Recognizing that line earlier would’ve saved me months of discomfort and frustration.
When Home Treatments Stop Working
I tried every home remedy consistently for weeks. Salt water gargles, water flossing, improved oral hygiene, dietary changes – all the recommended approaches. Some stones came out, but new ones kept forming faster than I could manage them.
This pattern of constant recurrence despite aggressive home treatment signals the need for professional evaluation. You shouldn’t be fighting new stones every few days indefinitely.
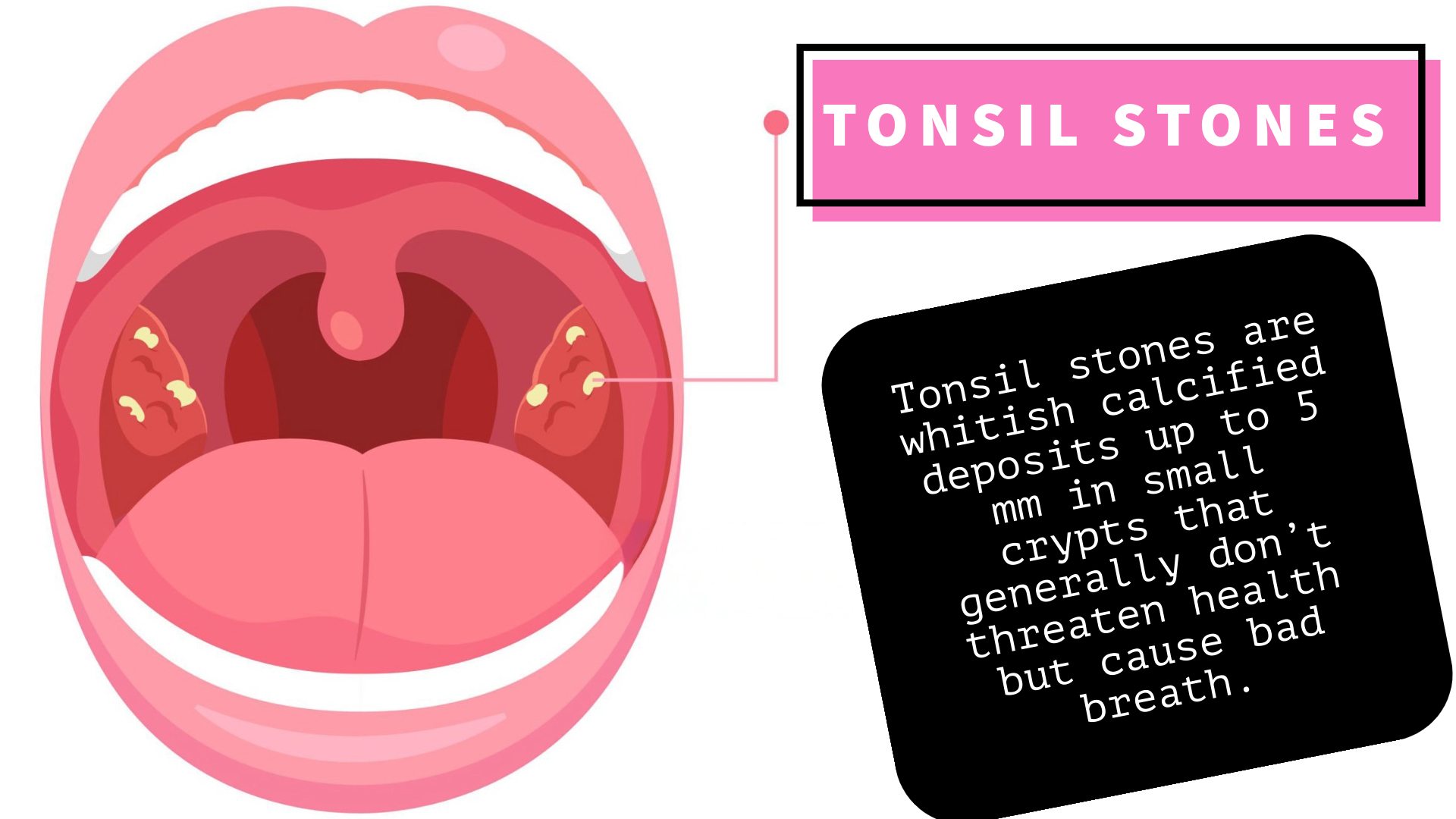
The stones also started getting larger. Early ones were small, maybe 2-3mm. But later stones reached 5-6mm or larger, too big to dislodge with water flossing or gargling. Size progression despite treatment is a red flag.
I developed resistance to continuing treatments that clearly weren’t solving the underlying problem. If you’re doing everything right and still struggling, professional intervention makes more sense than just trying harder with the same approaches.
Pain That Interferes With Daily Life
Discomfort is normal with tonsil stones. Actual pain that affects eating, drinking, or speaking means something needs medical attention.
I reached the point where swallowing hurt enough that I avoided eating. Lost five pounds over two weeks because meals became unpleasant. That’s not managing a minor annoyance – that’s a problem requiring intervention.
The pain radiated to my ear on one side. Referred ear pain from throat problems is common, but it’s also concerning. It suggested significant inflammation or infection beyond simple stone presence.
Sleep disruption from throat pain became constant. Waking up multiple times nightly because your throat hurts affects everything – work performance, mood, relationships. Quality of life matters, and chronic pain deserves medical evaluation.
Signs Of Infection
Tonsil stones themselves aren’t infections, but they can lead to infections. I noticed my tonsils becoming increasingly red and swollen beyond what the stones alone explained.
Fever developed – low grade at first, around 99-100°F, but persistent. Combined with throat pain and visible inflammation, this suggested bacterial infection requiring treatment beyond home remedies.
White patches spread across my tonsils beyond just the stones. This indicated possible strep throat or another infection needing antibiotics, not just mechanical stone removal.
The lymph nodes in my neck swelled noticeably. You could see the bumps under my jaw, and they hurt when pressed. Lymph node involvement means your immune system is fighting something significant.
Bad breath became truly awful despite obsessive oral hygiene. The smell suggested bacterial overgrowth that home treatments weren’t controlling. Professional cleaning and possible antibiotics were necessary.
Breathing Difficulties
My tonsils swelled large enough to narrow my airway. I could feel them touching each other when I swallowed, and breathing felt slightly restricted especially when lying down.
Sleep apnea symptoms started – my wife said I was snoring loudly and sometimes stopped breathing briefly during sleep. Enlarged tonsils blocking airways during sleep is dangerous and requires medical evaluation.
The sensation of throat closure during swallowing scared me. Not actual choking, but the feeling that swallowing was difficult enough to potentially become dangerous. That fear alone warranted seeing a doctor.
What The ENT Specialist Did
The ENT used a scope to examine my tonsils more thoroughly than I could see in a mirror. Revealed multiple deeply embedded stones I had no idea existed, plus significant inflammation.
Professional removal using specialized tools cleared stones I couldn’t reach. The instruments access deep crypts safely without causing damage or triggering excessive gagging.
The doctor prescribed antibiotics for the secondary infection that had developed. Home treatments don’t address bacterial infections requiring medication.
We discussed long-term solutions including potential tonsillectomy. While not immediately necessary in my case, having that conversation helped me understand the full range of options.
The specialist also identified contributing factors I’d missed – chronic post-nasal drip from allergies creating perfect conditions for stone formation. Treating the underlying cause reduced recurrence dramatically.
Medical resources like the Cleveland Clinic’s tonsil stone information explain when symptoms warrant professional evaluation rather than continued home treatment attempts.
Tonsillectomy Considerations
My stones weren’t severe enough to justify surgery, but the ENT explained when tonsillectomy makes sense. Chronic recurrent stones despite aggressive treatment is one indication.
Tonsils causing breathing problems, especially sleep apnea, are strong candidates for removal. Quality of life and health risks outweigh the benefits of keeping problematic tonsils.
Repeated infections beyond just stones – multiple cases of tonsillitis annually – justify removal. Your tonsils should protect against infection, not cause it constantly.
The surgery is more difficult and painful in adults than children. Recovery takes 2-3 weeks with significant throat pain. It’s not a casual decision, but sometimes it’s the right one.
My doctor recommended exhausting conservative treatments first. But knowing surgery exists as an option if needed provided peace of mind.
Specialized Cleaning Procedures
The ENT performed a procedure called laser cryptolysis – using laser to smooth out the deep crypts where stones form. Less invasive than full tonsillectomy but addresses the structural problem.
Some doctors offer coblation cryptolysis using radiofrequency energy. Same concept – reducing crypt depth means fewer places for stones to form.
These procedures are done in-office under local anesthetic. Recovery is minimal compared to tonsillectomy, maybe 3-5 days of throat soreness.
Not every patient is a candidate – depends on tonsil structure and stone severity. But for moderate cases, it’s a middle ground between endless home treatment and full surgery.
Ongoing Monitoring
Even after professional intervention, I need periodic follow-ups to ensure stones don’t return or underlying issues don’t worsen.
The ENT checks for new stone formation and evaluates whether the treatments are working long-term. Catching problems early prevents them from becoming severe again.
We adjusted my allergy treatment based on how it affected stone recurrence. Medical management of underlying conditions is ongoing, not one-time.
Having a specialist familiar with my case means faster help if problems recur. I don’t have to start over explaining history each time.
Wrapping This Up
Professional help becomes necessary when home treatments fail, pain interferes with daily life, or complications like infection develop. Recognizing these signs early prevents unnecessary suffering.
ENT specialists have tools and expertise that safely address problems beyond home care capabilities. Professional intervention isn’t admitting defeat – it’s getting appropriate treatment for your situation.
Don’t suffer for months trying home remedies that clearly aren’t working. Medical evaluation provides definitive answers and treatment options you can’t access yourself.
Most cases don’t require surgery. But knowing the full range of options from conservative treatments through surgical intervention helps you make informed decisions about your health.